Hospice chaplains are key members of each hospice team. What is their role, and how do they impact the dying and their family and friends? Ellie Douglass sums it up like this: “So much of our job is providing that space of being with suffering and being present and listening. Really providing a compassionate container for individuals as they are at the end of their life.”
instagram.com/artoftransitions
Transcript:
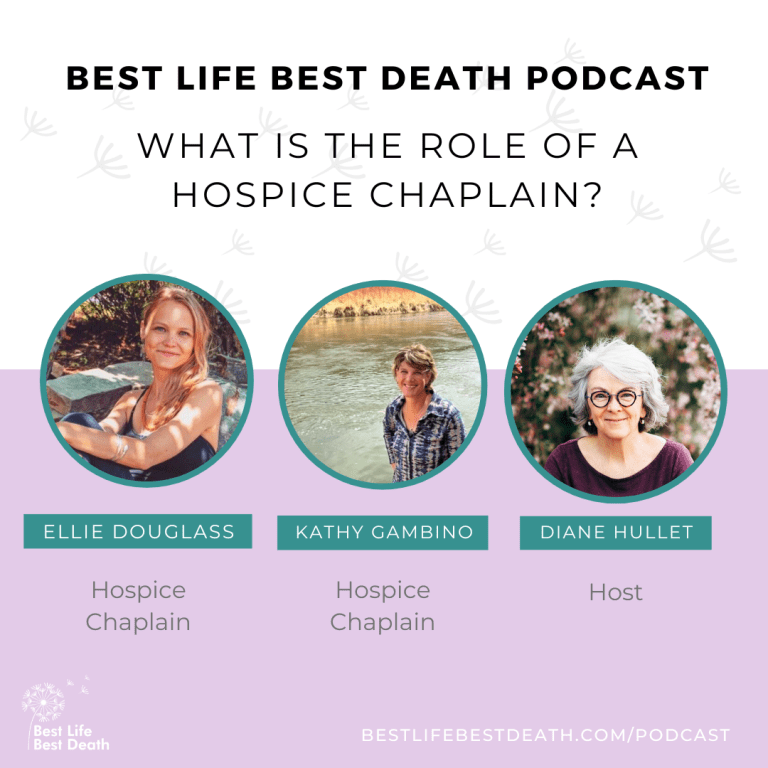
Hi, I am Diane Hullet and welcome to the Best Life Best Death podcast. Today I’ve got this really interesting combination of two hospice chaplains. So welcome. Welcome to Ellie Douglas and Kathy Gambino. Thank you. Thanks Diane. Thank you Diane. Yeah, I’m excited they know each other through the whole hospice world of Boulder, Colorado and Denver, Colorado.
And I know them both separately and then I thought, well, wouldn’t it be interesting to have two chaplains and just kind of talk. About what is the role of a chaplain, because I think sometimes people think it’s this very religious thing and if they aren’t religious, they might say, oh, I don’t need a chaplain.
I don’t wanna talk to that person. But I personally have found in my experience with hospice and family members, that the chaplain plays this kind of really beautiful role that I think is powerful. So let’s just kind of start with, why don’t each of you just kind of talk a little about what got you started in this work?
I’m, I’m happy to begin. So I, I grew up with a very spiritual mother and a father who was very open. And so when I was off on my own and went to college, I really started to study and look into different faith systems and became really curious and I started studying Buddhism. And so Buddhism plays a huge role in what led me to want to care for people at the end of their life.
I traveled to India and my experience there was really pivotal for me wanting to get my Master’s in divinity. And that’s also a really beautiful thing that Kathy and I share is that we both got our master’s in Divinity at the same place at Europa University. And there is where I, we, we both began to study how to really provide spiritual support for people at the end of their life.
I love that. Just naming it as like spiritual support. And did, did the two of you know each other when you were in Naropa? Mm-hmm. Yes. Nice, nice. Kathy, how about you? What, what brought you into this? Oh, I was a hospice nurse. That’s my background. And I was a nurse for 24 years and then was a hospice nurse for eight of those.
And during that time, both my parents got ill with. Terminal illnesses. And so I had the good fortune of helping care for them. And after they passed, I had like an existential crisis about death, and I wanted to know how to be with suffering. And ’cause as nurses, we, we are trained to fix things, right?
Or, or, and to help comfort people make sure they’re comfortable at the end of life. So I wanted to do a deep dive into how to the spiritual side of death both as a healing journey and how I could take that journey deep. For others. So I went from a role of nurse where you do with four people and with people to a role where I felt I could be with people at the end of their life and with what, whatever that looked like and however that presented.
Wow. I, that’s so, that’s very Buddhist, right? The be with suffering is really different than trying to fix the suffering. Yes. Mm-hmm. And so, master’s in Divinity, is that pretty typical of a hospice chaplain that they have that training? Yes. Traditionally, that’s what’s looked for in most hospices. A master’s in Divinity.
There’s also, you could have a master’s in pastoral education or pastoral counseling. That’s also, I’ve seen chaplains who offer, have that degree and then others. Ellie, I’m curious who, what you’ve run into. Yeah. Others will be in seminary, but every, every chaplain has to also go through pastoral counseling training, which includes an internship, whether you’re at a hospital or with a hospice or even military or disaster relief Chaplains.
So they want you to have your field experience before you truly enter into the, the field as well. That makes sense. And, and does every hospice have a chaplain? Yes. It’s required. It’s part of a Medicare requirement to have a chaplain or I think they sometimes say pastoral counselor in the Medicare regs.
So yes, it’s part of the inter interdisciplinary team that’s social. Social support. Can you say a little bit about that team and then say a little bit about when your piece steps in with a family, what do you typically do? Yeah, I mean, I think it’s quite incredible that the spiritual part is part of the regulation for hospice care.
You know, it’s, it’s holistic care and so when we’re caring for someone at the end of their life, we’re caring for the physical. You have your nurse the emotional social worker, often spiritual chaplain then you have your caregivers and your doctor and a whole team. It takes a whole team to provide that holistic whole self-care and oftentimes, A chaplain is a spiritual companion.
If someone is religious, then we provide that coordination with churches and, and the people that they want by their side. But so much of our, our job is providing that space of being with suffering and being present and listening and really providing a compassionate container for individuals as they are.
At the end of their life and asking bigger questions and being faced with fear and wanting to help cultivate a sense of peace for them. Beautiful because so much what I hear people talk about is a fear of death and a fear of dying, and a fear of suffering. And you’re really talking about how in your role can you help create this compassionate container that can hold all of that?
And, and so Kathy, why don’t you speak to like, what do you typically, how do you step in? You show up at someone’s home, or you show up at a hospital? Sure. And I so appreciate it. Wanna circle back to what you said at the beginning, Diana, how some people hear, Ooh, chaplain and, oh, I’m not religious, or, Ooh. Or some people, the word chaplain can be a little bit loaded depending on people’s religious, spiritual, or just life experience and their history.
And so when I, when I, what, what I usually do is the, the admission nurse will ask the family, Would you like a chaplain as to be part of your team? ’cause they have a choice. They can choose to say no to a chaplain or a spiritual care provider. They can say no to social worker. They can, they, this is about the family and what they need and the patient, what they want, and honoring them.
And just walking alongside that. So someone gets admitted to hospice, they’re asked if the chaplain could reach out to them. And if they say yes, I’ll call them and introduce myself. And just say, you know I’m just here to let’s say I’m talking to a daughter. I’m just here to meet your, your mother where she is.
I have no agenda. I’m just here to be a support and walk alongside you and be of any help I can and, and then ask can set up and meet with them. So it’s kind of defining that role, like Ellie said spiritual companion, like we walk alongside them. We don’t, I, when I go out to see a family, I do not have an agenda.
My whole purpose is to meet them where they are to build rapport, just to hold space for whatever is going on with them and just be with what, and allow whatever is happening to them and just be with them with whatever’s happening in that day, in that moment. And then reflect back to them, you know, if, if that, if it is a topic, they may be talking about their dog or their grandchildren.
So it’s really just whatever’s meaningful to them for me is what’s considered spiritual, religious. And it could be the Broncos, it could be their dog. So it just being with whatever is most important, and I usually ask when I do meet this person the first time. What’s most important to you these days or right now?
So I, ’cause I really wanna know where are they right now? ’cause they may talk about their career or their past, which is beautiful and meaningful in terms of life review. But I really wanna have a sense of where are they right now? What’s most important to them right now? And it might be spending, they might say, spending time with my daughter.
Then I know what’s most important to them so I can support whatever that is for them. I love this broad kind of definition of, of spirit really being about life and what’s important. And I, I reflect back on my own experience with my mother-in-law when my father-in-law was dying. And I remember her saying, oh sure, social worker visit, bring him on Chaplain.
Let’s see what they have to say. And I remember thinking, oh, chaplain, like, they’re not particularly religious. My husband and I weren’t particularly religious and so. I loved her openness to it. She just wanted to know what did hospice have to offer? And the chaplain who came was remarkable. And after about three meetings with her, I remember saying to her, how did you get this job?
I think I want this job. But she did. And so in the back of my brain, for a long time I thought maybe I’m getting a master’s in divinity someday. Like, who knew? But the, the value that she brought in just sitting with us and hearing what was happening and hearing what was important, I, I just never thought that that was, I think I was one of those people who had kind of this chaplain equals, priest equals, yeah.
Religion or something. I don’t, I don’t know. I just didn’t understand the, the depth and the breadth, and so I love how you’ve both brought that forward, this compassionate container and what’s most important. And, and I’m guessing the two of you must see just like the gamut of people. I mean, what they, what they say is important and what they say matters and what their connection is to their own spirit is, is probably remarkable.
Yeah. It truly is. This. At times I’m like, I can’t believe this is a job and this is my work that I get to show up, meet all these different incredible people, and really like enter into these spaces of awe through how resilient people are, how open they are to talk about their life at the end. There is a sensitivity and a, a tenderness always.
That we meet over and over again, resilience and oh, what gorgeous words. And, and Diane, there are people who can’t speak, you know, like people with say Alzheimer’s or people who are say in their last two weeks. And it’s such an honor and a privilege just to hold space for them just to be with, be silent, you know, even people with Alzheimer’s who may be walking around and talking just energetically.
Them know we are with them in that moment and finding some connect point that may not be words, and it may just be bringing a sense of comfort or peace while sitting next to them. So it, it can also be nonverbal. Probably mostly it’s nonverbal. I, I always am struck, I go back to Barbara Carns, you know, great end of life educator in her statement.
We don’t, people don’t die like they do in the movies. And now, almost every time I see someone die in the movies, I think I. That’s not really how it goes like that. You, you, you look good and you’re talking and then you just are passing. It’s like, it’s, it’s a process and I think the body has to labor to die in many cases.
Obviously not in sudden deaths and so on. So your role as chaplain is part of that labor and that takes time and a lot of it is nonverbal. Yeah. Just being comfortable while the body is shutting down. You know, that labor part is also important. Helping educate the family what’s happening and normalizing the process.
’cause it can be scary for people who’ve just seen it on TV and it’s their first experience. So that’s a piece of it too. Hugely scary and huge education. And in that regard, you’re kind of just another voice in the hospice team of educating, right? Yeah. Mm-hmm. Ellie, what were you gonna add? Oh, well, I mean, I guess just to add onto that, so much of our job is normalizing this human condition and the dying process.
And it helps relax the individual knowing what may happen or what is happening or that that sound or that breathing pattern is okay. And one of the most beautiful aspects of. The dying journey that I found is that oftentimes there’s this moment of lucidity that can happen and educating the family members that that lucidity might show up during that process of dying helps the family be aware and attentive to that moment showing up.
I remember telling a family member about this, and we used Barbara’s book booklet all the time. Gone from my side. And that is a huge aid in helping to educate people about dying. But he had a moment with his father before he entered into his dying process where he had dementia and he had this clarity come to him and he talked about his life with his son and how much.
He’s gonna miss his grandchildren, what he wants to pass on and, and then his son knew that he was in that moment of clarity because of our education. And then he had a few days later entered into his dying process. Beautiful. So education can really assist and having the family members be really present, have them be sort of ready for those moments and those both of lucidity and of.
Ending speaking or lucidity. I remember also reading a book where the man’s wife had, had you know, begun a dying process and, and he said, you know, he was sort of like, oh no, that was our last conversation. Like, I didn’t know. That was our last conversation. So how do you prepare for those kind of transitions that are shocking and they’re coming and it’s.
Best if you’ve got someone really supporting you in that, which, which makes me think about how key the hospice role is for the family, almost more than the dying person or equally important to the dying person. Would you agree? Yeah. We always say that we are here for the family as much as we we’re here for the patient.
Yeah, it’s one unit of care and their family members are not separate from the patient and. How they’re cared for affects the patient. You know, oftentimes people are worried or feel concerned for those that they’re leaving behind. You could say it’s often, there’s so many opportunities for just.
Everyday rituals to, to do with the family to help them either say goodbye to their loved ones. You know, gathering, looking at pictures, just most natural, everyday having family gathering in a meal together. So there’s also the, along with the suffering, there’s also like this celebration of their life.
And we often encourage families to do kind of a life review with their loved one, because that seems to be. Something that’s really helpful to someone, for someone to pass. It’s almost over the years of my experience, almost like a prerequisite in some way. And so that can be done looking at photo albums that can be done, having a little party that can be done, whatever’s authentic and meaningful for the family.
And often that piece at the end of giving permission to their loved one is huge. Where we work with the families in, in whatever way is natural to them, helping them. Say thank you or goodbye in whatever way again is natural for them because that piece, ’cause often the person dying is wanting to make sure that whoever they’re leaving by behind is okay.
You know, that’s their part of that letting go. And so we work with families all the time about that piece of hospice and telling, you know, the person you know, all your business affairs are taken care of. You know, we’re gonna take care of each other. You don’t have to worry about anything. You know, your work is done here.
And that piece Diane is so huge and families helping their loved one pass and us helping the families help their loved one pass. So that’s a good piece. I can feel that, like, I can feel that, that if you, if you can truly take that in and you feel that your loved ones are okay, as you said, quote unquote, okay, then there is this restfulness, like you can just sink back into.
I imagine the agitation of, if you don’t feel that way, if there are unresolved issues, you know, which, which is sort of what I love about the best life, best death, right? Because I think when we connect with our best death, it does bring us into our best life. So, If there’s some unresolved thing you wouldn’t wanna have on your deathbed, is there a way to move it forward?
Now, you know, not that everything’s neatly resolved, but the things that hang over us as these, these burdens stay with us until the end. And sometimes there’s a way to make a shift. Sometimes there’s not. But boy, if there is, what, what that might look like and how that changes the, the end game for being able to let go.
So the two of you, you, you really swim in these like big areas with people. It’s so beautiful. I imagine you being out in these deep ocean waters with people, you know, you’re not in the shallow end of the pool. Yeah, yeah. What, what do you feel like, are there things you would wanna say to people, to listeners about hospice that you feel like are important to know?
Little nuggets. Well, I know we’re talking about chaplaincy here and we’re talking about spiritual care. And so I think I always encourage the welcoming of the whole team. Like you said, your, your family member was like, okay, I’m open. Bring the social worker, bring the chaplain. I think that’s important.
And of course, everyone has their own autonomy and, and can choose who they want to have by their side during this intimate time. But so much of it is relationship building and creating a safe, loving container. It’s really beautiful that it’s a whole team of people that get to enter into your life.
Whether that team will be there just for the family or just for the patient or both. When you say the relationship piece reminds me how important it is that, how, how powerful it can be if you can call hospice sooner rather than later. ’cause I think sometimes people who are unhappy with the hospice experience, you know, they were with hospice for a week and they never saw the same nurse twice and the social worker never got there.
Well, there wasn’t time, there wasn’t time for this. Relational pieces. So I think about how do we, you know, encourage people calling hospice sooner rather than later. It, it’s not a death sentence. It’s a, it’s a lifeline, it’s a support, it’s ease for that transition and information for everybody. Yeah.
Yes. And that’s so true, Diane, you just Yeah, that is so true because it is about that relationship and. There’s a trust building, right? These people, we come into people’s life very vulnerable and intimate time. And so for us to get to know a person and the nuances of the family and dynamics and how we can best be sensitive and support them it happens so much better when there’s time for a relationship to be built.
And you don’t have to be, we have some people on hospice for two years. You, it, you don’t have to wait. Until the last two weeks. And there’s often a stigma related to it. And a lot of people who start on hospice get better because they have all this loving attention. And I’ll give a short example, a story about how team is so important.
And it turns out that we had a woman who couldn’t speak, who had Ms. Who we found out from the family member and they had, they knew how to communicate with her that she wanted before she died. She wanted to smoke a cigarette, have a drink, and be around a handsome man. So we happened to have a male volunteer.
And so this is, this goes to show you that because we had been caring for her for over six months, we. We, we were able to do this with the family that we as a team threw her party. She was a French teacher. We threw a Paris party, we decorated the room in everything Paris. We had a volunteer male who at the end of the party, she kicked us all out ’cause she just wanted to hang out with him.
And she, she winked me to let me know that we had made a good choice. So it can be that simple where it really is the whole team and just finding out like what would be important to her. And that brought her a lot of joy and she passed away a couple days later. So again, just an example of how, it’s the whole team, including volunteers.
We have amazing volunteers. Right, who can really kind of bring this time to what have you said at the very beginning, something about how do we make this positive and peaceful? You know, that I, I think some people are shocked even to hear that that’s an option. Yeah, it’s certainly possible. I think we all, we all want that, you know, so how, how can we help facilitate that for another and that’s such a beautiful story, Kathy.
I love it. You know, that’s, that’s what. That’s what it’s all about. It’s, and having someone on hospice for longer than a week you get to really know what their wishes are and yeah. Know that she’s a, was a French teacher and she would wanna party. Yeah. That’s beautiful. You have both worked for different sizes of hospices, is that right?
Are you currently working for a little one? A big one? A medium one, yeah. For a little while there Kathy and I worked for the same hospice but I’ve worked for, for multiple and they’ve grown and. And now I work for a small hospice, which I truly enjoy most, and I think it’s my final hospice that I’ll remain at for a while.
But there are different sizes and I think that having a small hospice is wonderful and provides really intimate care and consistent care too. ’cause sometimes when it’s really big, things can fall through the cracks. There’s lots of different hospices out there. Yeah, I think there’s benefits to both.
I work for, we, I think the hospice that I work for has about 200 patients and has enough teams to support those patients. Geographically, there’s, I think there’s like eight teams, depending. So however many people are in that area get cared for by 18. So I think there’s sometimes more infrastructure.
I, it really depends on the hospice. I think everyone’s intentionality is the same different hospices that they’re really there. We’re all really there to help our patients and families and support each other. Then of course, you know, sometimes when things get bigger there’s more layers of management, and so that can be a benefit and a a detriment.
So it, it really depends. But I think regardless of size, the intentionality is all the same from one hospice to another, regardless of size. You know what, but I really appreciate the fact that there’s a, at least working at a smaller one that has definite advantages. Yeah, I was thinking recently, I mean, if I had advice to give, I would say shop around before you need it.
Like keep your ear to the ground on what different hospices are like in your area. Because I do think they’re changing a lot currently. Like there’s a lot of, they change size and they change ownership right now sometimes rapidly. So I think you wanna kind of keep your ear to the ground about who is in your area, what they provide, what their.
References are like, before you really need it, you know, you don’t wanna have to call them because you’re desperate and somebody just took a turn for the worst and you don’t even, you’re in your own grief and you don’t even know what you want. So I always think about that, you know, get on it ahead of time.
And then I, I think we’ve also kind of had a nice thread of saying just be o be open. Be open to what they have to offer and all their services because sometimes the chaplain might play a role that’s, Even more touching and powerful in your family than you might’ve realized. Well, I thank you both so much, and both Ellie and Kathy worked for hospices, but you know, they’re not the be all end all.
So we, we kind of talked about, we weren’t necessarily gonna give websites for those, but look up hospices in your area. Reach out to me if you have trouble finding anything. And thank you both for joining me today and having this conversation about hospice chaplains. Yeah. Thank you so much, Diane.
Thank you, Diane. Thank you. You’ve been listening to the Best Life Best Death podcast. I’m Diane Hullet, and you can find out more about the work I do at Best Life. Best death.com. If you wanna reach out, find me there. Thanks for listening.

End of Life Doula, Podcaster, and founder of Best Life Best Death.