This episode is chock-full of important information about a topic that affects so many. What is dementia? What symptoms might it include? Why does it matter to test for dementia? What is a “dementia advance directive”? What are the needs of caregivers? How can support groups help? Jessica Empeño is the National Director of Clinical Engagement & Education for the nonprofit organization called Compassion and Choices. If you aren’t familiar with this key organization, search them up today. Their indispensable and free downloadable workbook on this subject is called the “Dementia Values and Priorities Tool.” Books we mention include: The 36 Hour Day; Care Boss; and The Best Friends Approach to Dementia Care.
For more information on Best Life Best Death please visit our website at www.bestlifebestdeath.com.
Follow us on our social channels to receive pertinent and helpful resources on death, grieving, and more at:
Facebook: www.facebook.com/bestlifebestdeath
Instagram: www.instagram.com/bestlifebestdeath
Transcript:
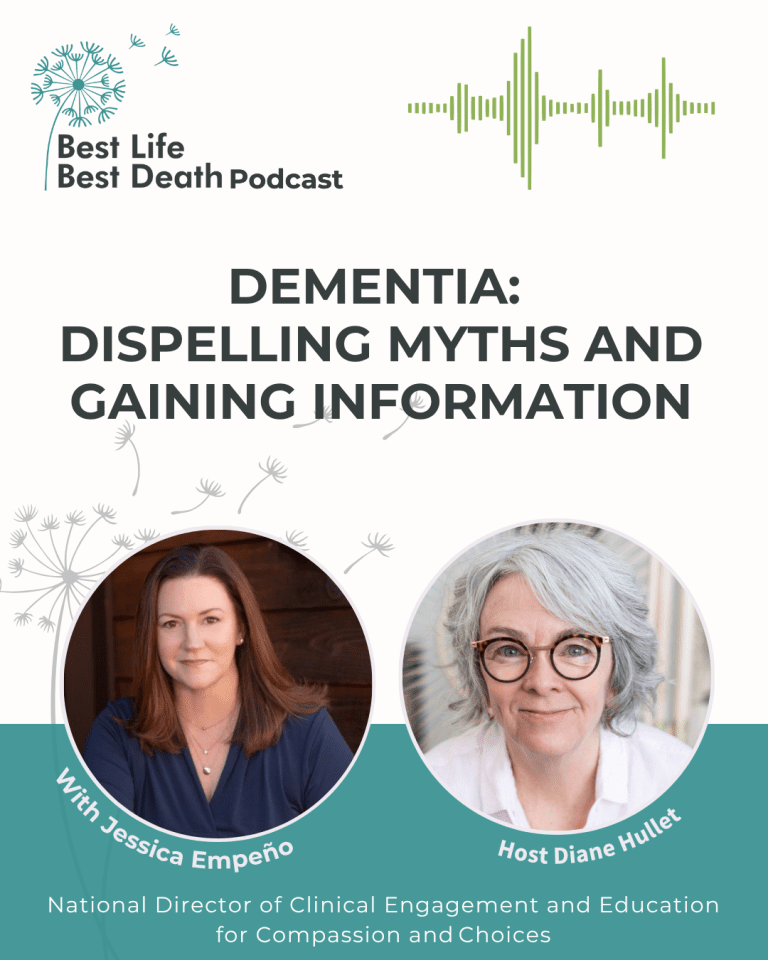
Diane Hullet: [00:00:00] Hi, I am Diane Hullet and you’re listening to the Best Life Best Death podcast. I’ve got a repeat guest today, which I’m very excited about. Welcome to Jessica Empeño.
Jessica Empeño: Thank you so much. I’m thrilled to be here.
Diane Hullet: I am delighted. So, we talked back really fairly recently on podcast Best Life, best Death Number 2011.
No, I said that wrong. Number 211 talked with Lisa Paul and Jessica and Peno of the death deck. I think I said 2011. ’cause that’s just like my dream that there’s 2000 episodes out there. Right. But we’re, we’re gone over 200 here and it’s, it’s, it’s a really good time to be having these conversations and bringing these topics forward.
So Jessica, you and Lisa, Paul and I talked about the dementia deck, which is this tremendous new tool to use for talking about dementia. And when Lisa and Jessica and I got off the phone, I said, Jessica, we could talk more about this. I have a feeling ’cause it, it’s just dementia is such a big, big subject.
So welcome back. [00:01:00] Thrilled you’re here. And why don’t you just tell people your title and kind of how you do your work and how you got into it.
Jessica Empeño: Thank you Diane. I’m so glad to be here and I was so grateful for your invitation to talk more about dementia because this is such an important topic and it’s one of those things that affects so many people and the opportunity to help answer some questions, maybe dispel some myths.
Has actually been a really big part of my work as a medical social worker for a lot of years. So I’ve been practicing for about 25 years and I have worked primarily in end of life care and in dementia care, supporting people living with the disease and their care partners, but also supporting professionals to help them build their knowledge and understanding.
Of dementia and how to support people in the community that are impacted by the disease. So I joined the team at Compassion and Choices as the National Director of Clinical [00:02:00] Engagement a little while ago, about two and a half years ago, to be able to take that work and really worked toward.
Advocating for change improving care supporting access to the types of supports and services and care that people deserve and, and need at the end of life. And dementia plays a really big part in that because we know that there are a lot of adults that are living with dementia at the end of their life.
Diane Hullet: Yes, and I don’t have any like statistics to pull out. That would’ve been a good thing to prep ahead of time, but you do. Oh, good. Do you have any statistics at your fingertips? I do, yes. How many people are living with this? What? What’s happening?
Jessica Empeño: So our best estimates are that close to about 7 million people in the United States are currently living with some form of dementia.
And we’ll talk more about what I mean by that in just a second. But this is a disease where those are the, those are the people that we know about. Those are the people that we can [00:03:00] tell from their records where it was clear that they had this diagnosis. My theory is there are far more people living with some form of dementia that we know about because either they didn’t get a diagnosis.
Because maybe their medical records weren’t clear. Maybe the death certificate as it was filled out didn’t include that they had Alzheimer’s disease, for example. So I think this is something that affects far more people. But one of the other things that we do know is that almost half of older adults have some form of dementia at the end of their life.
That’s a lot. But again, those are the ones we know about. So I think it’s a lot more than that.
Diane Hullet: That’s a lot. That’s really a lot. And, and say a bit about, I mean, you kind of alluded to this, there’s so many different types of dementia and there’s so many different sort of stages and places that dementia shows up.
Give us, give us a little big picture overview of what we’re even talking about. [00:04:00]
Jessica Empeño: Yeah, this is a really important place to start because although dementia is, you know, this term, that kind of gets used a lot. It’s, it’s shared as a diagnosis, right? People will say all the time, you know, my, my person has diagnosis dementia.
That’s incomplete. So dementia is a general term to describe a collection of symptoms, which are different for every person, particularly depending on the cause of those symptoms. And there are over a hundred different types and causes of dementia. And so dementia, I think it’s important to know isn’t just about forgetfulness and memory loss.
For some that is a very classic, oftentimes the very first set of symptoms that they experience. But for many, it’s more than that. Dementia will affect personality and behavior. It impacts language and communication, [00:05:00] judgment and decision-making, even physical abilities and our senses. Really, it’s how the brain sees and.
Make sense of and interprets the world. And when that changes for a person that changes the reality that they live in, that changes how they function and their safety becomes a concern. So there’s a lot of things that are impacted by somebody living with dementia.
Diane Hullet: Wow, that’s such a really strong, big overview.
And of course, the impact on the people they live with or the impact on their caregivers or their adult children if they have them or their community in terms of how they’re cared for. Right? S setting care, caretakers, caregivers, care providers aside for a minute, let’s talk a little about, you know, about testing.
I hear people talk about, well, maybe should you test for dementia? Do you not test for dementia? Can you get a test where you live? [00:06:00] Can you not access a test? What, what does, what does testing get you, and why would you test?
Jessica Empeño: Such a good question. This is a question I hear from families a lot. I think there are a lot of fears.
You know, testing can be scary. You know, a lot of people will say, well, I, I don’t really wanna know, or what doesn’t matter anyway. Or they might fear what happens as a result of potentially receiving a diagnosis. Right. I’ve had people say that they, they don’t want to talk to the doctor. They don’t wanna get a diagnosis because, well, they’re, they’re gonna take my car keys away.
It’s not quite that black and white. It’s important to know, though. I think that there are many different types and causes, like I just said, of dementia, like symptoms and some of them. Can be reversible, right? So if somebody is dealing with medication interactions can cause dementia like symptoms, things like [00:07:00] hydration, vitamin deficiencies, and malnutrition.
But in older adults, particularly a very common cause of dementia like symptoms is depression.
Diane Hullet: Amazing.
Jessica Empeño: That’s, and a lot of people don’t realize that, you know, in younger people, depression looks more like, I think the sadness that we tend to think, right? That feelings of hopelessness, feelings of helplessness.
But in older adults, depression can show itself as forgetfulness as. Confusion being disoriented, not being able to, you know, process and think about things the way that they used to. So I think it is really important to find out what you’re dealing with because what if it is reversible? What if there is a potential treatment that could help somebody restore their level of functioning?
Now there are causes of dementia that are not curable, like frontotemporal dementia. Lewy [00:08:00] body Alzheimer’s disease is the most common cause of an incurable dementia. And so it’s still important to know because. If you’re going to start, let’s say medications, there are certain medications that you don’t want to be taking depending on what type of dementia you’re living with.
So it can also be a safety issue. So getting a clear diagnosis, understanding what’s really going on is absolutely worth the time. It can be hard. There’s not one clear test that you can take. It’s, it may be an arduous and. I need a long extended process to get that diagnosis, but I’m an advocate for, for giving it a shot.
Diane Hullet: What kind of place where do you even begin to get a test?
Jessica Empeño: The best place to start is with your physician. Start with your physician and say, you know, this is what I’m noticing. This is what I am experiencing. The, one of the keys is a [00:09:00] dementia is going to be something that you see gradually over time.
It’s not going to be one of those things where it’s like, you know, all of a sudden. This is what’s happening. If, if that is what you’re seeing, if it’s kind of like an all of a sudden sort of thing, like a week ago she was fine and now she’s, you know, so confused. That could be a sign that we’re dealing with something that could be reversible, like say a urinary tract infection, right, or a medication interaction.
With dementia and these changes that we see, they come on slow over time, and it’s almost like looking in the rear view mirror. Then you realize, you know, a couple of years ago, yeah, things were a little bit different. So starting with the physician and being as specific as possible about what you’re seeing and what your concerns are is a really good place to start.
Sometimes the physician will be able to coordinate the testing process, and sometimes they might refer you to a specialist, but because there isn’t just one test, [00:10:00] you know, if somebody receives just that pen and paper, draw a clock, spell world backwards, that’s incomplete. You need much more than that. We need blood tests, we need scans, we need other things to rule out these other potential causes.
Diane Hullet: Amazing. I think that’s fascinating that depression in older adults can be a piece of a level of forgetfulness and and disengagement. Even that then, if that’s what’s happening, you wanna know that right. And figure that out because there may be some support for that.
Jessica Empeño: Exactly. And a lot of people don’t realize that somebody can have both.
Right? You could be living with depression and dementia and one will just keep making the other worse. So treatment is important.
Diane Hullet: What I’m struck by for, you know, people listening, what I’m struck by is, so maybe you’ve got an aging parent or an aging beloved aunt or uncle or a friend who you consistently help [00:11:00] and you might be seeing these things or an a spouse, and yet both of those words are big words for people to say, you know, I’m concerned you’re depressed, or I’m concerned you have dementia.
Any tips for how people might approach this? Are people generally in your experience, open to being tested?
Jessica Empeño: Yeah. This is where that things definitely do get tricky and what I have always advised families is if this is something you’re concerned about and somebody you love, you know them best. Think about what approach you think would reach them, but you can’t be afraid to talk about it.
These can be hard things, but you can’t be afraid to bring it up because if you don’t, it could definitely get worse. Right? And safety could be at risk and you don’t want, you know. To be regretting that you didn’t bring it up sooner.
Diane Hullet: Mm-hmm.
Jessica Empeño: So you can ask things like, I’ve noticed [00:12:00] this. We wanna try to do things that maybe don’t put them on that kind of defense.
Right. To say I’ve sometimes it helps to make it about you. I’ve been thinking about this. I wonder if you’ve been thinking about this or I’ve been feeling this way. I wonder if you ever feel this way too. I would like to go have a memory screening. You know, I’ve, I’ve, it’s, I’m, it’s about to be my birthday and I think this is just a good thing to do as part of my annual wellness check.
Side note, it should be done as a part of the annual wellness check. But sometimes making it about yourself can be helpful if you have somebody that is resistant. So try different ways, and if one thing doesn’t work, don’t feel like it’s off the table. Try again.
Dianne Hullet: Or, or you have a conversation, it’s a good conversation, but then the person forgets you had the conversation.
That’s that’s very, very real too.
Jessica Empeño: Exactly. Exactly. And if you have [00:13:00] somebody that you know, they’ve already experienced a number of cognitive changes and maybe they aren’t able to understand and process information the way that they did before. Maybe we don’t need to lay out every fact, right? Because sometimes arguing with logic isn’t what’s going to work, right?
So maybe we just say, Hey, it’s time for a doctor’s appointment. Time to time to go get a checkup, right? Almost, almost no big deal type of a type of a thing. Because the important thing is getting them there. What I also tips I give the family too, in addition to being specific, writing your concerns and your questions down to help prepare for that doctor’s appointment is sometimes it helps to call the doctor’s office ahead of time and explain why you’re bringing your person in.
What you’re noticing, what you’re concerned about. And that way you don’t necessarily have to go into all of that while that person is there. It kind of honors their dignity a little bit, but [00:14:00] you have that chance to share in confidence what your concerns are. So hopefully the doctor will pick up on your hint and be able to watch for those things as well.
Diane Hullet: Right. And I guess with HIPAA you can call a doctor’s office as a concerned. Person and give information. You can’t get information back unless you’ve got that legal ability to get the info back. Right.
Jessica Empeño: Yeah. Sometimes that will work. And sometimes they won’t even want to receive information from you unless you have that authorization.
So it may depend. But hopefully you know, those. Those are if you don’t have already. In addition to advanced directives and planning for future healthcare decisions, make sure you have those things in place so that the doctor’s office knows who those important people are and who they do have the authority to speak with.
Diane Hullet: Ooh, let’s underscore that, right? It’s so important to review your important paperwork. Have the right people in place to be medical power of attorney, decision makers, [00:15:00] whatever it’s called in your state, who speaks for you when you can’t, and also financial. And that makes a really big difference, doesn’t it?
Jessica Empeño: Absolutely does. It can’t underscore enough the importance of not only completing those important legal documents, sharing them with everybody, don’t feel like you need to keep them locked up in a secure place. Everybody needs a copy of those. But also the thing that’s even more important than filling out those papers is having the conversation.
Talking to the person that you’re choosing as your healthcare proxy or your agent, and making sure they know what your wishes are, what your preferences are, so that when the time comes, they know how to make decisions on your behalf and they know how to honor your wishes. That is the number one most important thing.
I would say when you go to that doctor’s office, and mind you, this could be your physician’s assistant, your nurse practitioner you know, when you’re having those conversations with your [00:16:00] healthcare team, if they don’t bring it up, it’s okay for you to bring it up to say, I would like to discuss. What my wishes are, I would like to share my advanced directive with you and discuss it.
I might even wanna have a conversation about filling out a post, so don’t be afraid to bring those things up to your healthcare provider so that they know what’s important to you as well.
Diane Hullet: Wow. Good advice. And also, we were talking before we hit record just about this intersection of end of life and dementia.
And I, you’re, you’re kind, you’re hitting on it now here with this, this piece of our advanced directives and conversations with those we love, so they know what decisions we want. But you know, just imagine listeners, it’s like, so maybe you’ve got some cognitive impairment kind of coming on over the last few years and now you are in a health crisis.
Which probably makes you more confused and more uncertain [00:17:00] and more reliant on the people who are your advocates, speaking for you, whoever that person is. So speak a little about that juncture or that weaving or, I don’t know what to call it, that collision course of dementia and end of life and crisis decisions end.
Jessica Empeño: Well, there’s so much we could say about this. You know, I think it is again. Aside from having those conversations and choosing someone that you trust and feel confident in making decisions on your behalf, talking openly about dementia, if this is something that you are diagnosed with, something you are concerned about, something you’ve had a family member with, maybe you also want to complete a dementia directive.
That is a special type of document that communicates your wishes if you are living with dementia. And it talk, it walks through some of those very specific things that you will see in the progression of the disease, and it’s a another way to include dementia in the [00:18:00] conversation. And Compassionate Choices offers a very unique type of dementia directive called the Dementia Values and Priorities Tool, which is available for free on our website.
It’s that tool for having that conversation because I think a lot of people don’t realize that dementia is indeed a terminal disease. If you are living with, let’s say, Alzheimer’s disease, Lewy body frontotemporal, this is not a disease that is going to be reversed and cured. So we need to plan. We need to plan for what’s coming.
We need to be able to talk openly about what to expect, and the more that the individual with the disease is able to share what their wishes are and talk about what they want for their final phase of life, the more they’re giving their loved ones that gift of being at peace of [00:19:00] knowing how to make decisions on their behalf.
Diane Hullet: And is the compassionate choices, is the advanced directive tool for dementia or the dementia directive on your website, is it tied at all to stages? I sometimes hear people talk about stages of dementia, and I think there’s an older model that’s like seven stages of dementia, and then there’s more, you know, tell, tell, tell us about stages and do they tie to the directive or no?
Jessica Empeño: Yeah, this is a good question. So yes, there is a step seven stage model that some people use, however, I don’t know about you, but trying to keep track of those seven stages and where people fall is a little complicated. So a lot of experts in the field really focus on the three stage model, which is early or mild.
Dementia, a middle or moderate, and then a late or end stage. The tricky thing about that is it’s not always this clear linear [00:20:00] progression. People have their ups and downs. They have their good days and their bad days. People who have been close to somebody with dementia knows that they could be clear and lucid and able to make their own decisions in the morning, but by sundown.
Right. They become a different person and they have a change in behavior and they’re not able to make decisions anymore. So it, it is tricky. But generally speaking, people in the early stages of the disease are still able to make their own decisions. They can sign legal documents. They may still be working.
Driving living their life, they may be able to continue living independently, but by the middle stages of the disease, which truly is the longest phase of the disease. That is when people will eventually require 24 hour assistance. They won’t be able to be making their own decisions. Safety becomes a concern.
So there’s a lot of of things happening in, in kind of that middle phase of the disease. Then the final stage is [00:21:00] where we really focus on the end of life. So for some people that could be the final months, it could be a final year or two of life. But by that phase of the disease, people pretty much are bedbound.
They are requiring assistance with all their activities of daily living. They probably don’t have a lot of intelligible. Speech left. And hopefully people are receiving the support of hospice or palliative care to ensure their comfort because by that time, a person isn’t going to be able to articulate their needs.
They’re not gonna be able to express being in discomfort verbally, at least. So we hope that they have that additional support. And like you said, the families and the caregivers and the care partners, they may not be diagnosed, but they sure are living. With this disease and there is a lot of information out there, there are a lot of resources and support that, you know, when you’re just trying to get through the day can be really hard to go out there and [00:22:00] research and find.
But I hope people will take advantage of the different programs that are out there because, you know, our, our, our goal is to really help people ride the wave without letting it crash over them. As they’re living with this disease. And so there are a lot of great places to go to get that support. But in the meantime, having those really crucial conversations at home together as a family to make sure that everybody’s on the same page.
Yeah.
Diane Hullet: Wow. Just, wow. I keep thinking the word. Wow. There’s gotta be a more interesting response. But I’m, I’m so struck by the way you’re laying this out and one of the things that we don’t really have time or the expertise to touch on, but I’m, I’m struck by the cost you know, not just in your own as a caregiver, your own time and lost work and so on, but truly the cost to society and how families.
Manage this is is pretty [00:23:00] stunning. And demographically, we’re heading into more and more people aging. Do you have any comments about that Broad, how expensive this is and how people cope with the cost.
Jessica Empeño: The research is, and the numbers are astounding of the true impact of the different types of dementia on, on our healthcare system, on our communities, but especially on families.
So we know that healthcare systems and insurance providers like Medicare and Medicaid are paying millions and billions of dollars every year to support the care of people living with dementia. We know that people with dementia often end up with more aggressive, sometimes even unwanted treatments in the final year of their life.
But what we have a hard time truly measuring is the impact on families, because the majority of the support and that 24 hour [00:24:00] around the clock care the help with, you know, just the normal daily activities, you know, housekeeping and meals and transportation and supervision so that somebody can go take a break or, or work while their person stays at home.
That’s not covered by insurance. That’s paid for by families. And a lot of families don’t have the type of money that it takes to be able to hire hourly help in the home. People are leaving their jobs or going part-time. So the true financial impact, I don’t even think truly honestly, that it, it can be measured, but we know it is significant.
Diane Hullet: Yeah. Let’s, let’s leave folks with some resources. Do you have any favorite let’s, let’s say the Compassion and Choices website and some of your favorite spots on there, but what other resources or books or websites or Yeah, what do you recommend looking into?
Jessica Empeño: Oh, there [00:25:00] are so many wonderful books and stories and memoirs written about life with dementia.
There are great resources for advanced care planning and, and having those conversations. So the compassionate choices, not only do we have the Dementia Values and priorities tool, which is that dementia directive I spoke of, but we also have the end of life planning and Decisions Guide, which is a workbook to help.
Walk people through, these are the things you might wanna think about. These are the things you might wanna talk about in terms of kind of those practical day-to-day, you know, help in the home, types of resources. We have a lot of people who served in our military. And their dependents, their spouses, A lot of people don’t realize that there are supports and services available through the va.
They have a caregiver support program. There are caregiver resource centers. A lot of county agencies on aging will [00:26:00] have. Supports. The Alzheimer’s Association, of course, offers many wonderful programs and a 24 hour helpline where people can call in and ask their questions and, and get more resources.
And then there’s a lot of really wonderful. Community programs. So in the community where you are speak with a social worker, talk to perhaps an end of life doula or your care team about the additional services that are available in your community, because there are a lot and if you haven’t heard of it already.
Be sure to look up the guide model. This is a pilot program being run by the Center for Medicare and Medicaid Services that is specifically designed to support people living with Alzheimer’s disease and their care partners. And there are hundreds of sites all across the United States that are offering this new innovative program and it’s.[00:27:00]
For the first time. It’s really exciting because it’s the first program out there to really give families the type of practical support that they need.
Diane Hullet: Do you think if you put into your computer the guide model, it will pop up?
Jessica Empeño: Alzheimer’s disease guide model, it will come up. There’s a website where you can search by your zip code and find a provider near you.
There are also some online telehealth providers like Ripple, for example, that are providing these types of services virtually. So there, there are a lot of options out there and it can be pretty overwhelming to try to navigate that system. But again. That’s what social workers, that’s what care managers, that’s what you know, nurse navigators.
This is what they specialize in. So don’t be afraid to reach out to them. They know what these resources are. Let them do that homework for you. Or next time somebody says, Hey, what can we do to help? Give them an [00:28:00] assignment. Tell them how they can help you. Go find me some resources.
Diane Hullet: Tremendous. I, I appreciate you noting that some of them are national, you know, which would, could be accessed internationally as well.
And some of them are really local. So what’s happening in your area? Do you live in a small town or a bigger city? And what, what can you find? Another piece that I’ll throw in is a book that I really love called The Care Boss by Jennifer O’Brien. And what I love about the care boss is that she really helps people break down what are all the tasks they’re doing as a care provider and what are all the tasks that they could maybe farm out to somebody else.
So seeing yourself as the boss in a role where you have to do some delegation and helping you figure out what can you delegate, what can you not? So it also pops in my mind to suggest to people. You know, we sort of alluded to this, but when you’re in the thick of it, it’s really hard to access this stuff.
So maybe if you see [00:29:00] something coming begin to kind of familiarize yourself with some of these aspects that maybe you can click into Ask Friends Talk. To people in your community, find a social worker you could rely on begin to tap into some of this so that a year or two, or three or four from now, you’ve got something dialed in.
I, I’m just struck by the burden on families. It’s really something and. Many, many people would say they don’t want this, but here we are. You know, the wonderful Western medical world has made it possible to take care of pneumonia and UTIs, as you said, and all these little secondary infections that used to kill us much earlier.
And so we live longer lives and often that impacts the way our brains are operating.
Jessica Empeño: Yeah, you’re exactly right. And you know, to that point, I would also encourage people to be open to the possibility of a caregiver support group. Whether that’s an online group, whether it’s in your community, caregiver support groups are an [00:30:00] amazing way to not only connect with other people who might understand what you’re going through in a way that others can’t.
Talk about an amazing place to get recommendations and resources and tips and tricks. That is such a great place. So I would encourage caregiver support groups and to add to the book recommendations. My favorites are kind of. Older tried and true books. I love the 36 hour day. I think that is a, it, it’s full of very practical information.
And my other favorite is the Best Friends Approach to Dementia Care by David Troxel. It’s been around a little while, but. In both of those books, the information I think really helps you understand what’s happening and maybe what’s behind a, you know, quote unquote challenging behavior that sometimes we see really understanding that, you know, sometimes people are doing the best they can with what they have and the [00:31:00] changes that they’re living through.
And I think when we. Have that understanding, we can have more compassion and maybe a little bit more patience because this is a disease that demands an incredible amount of patience and perseverance from caregivers.
Diane Hullet: Hmm. Beautiful. Well, thank you so much for joining me, Jessica. I think this is really, you know, we’ve said a lot for people to digest, but I hope folks found this helpful and you know, if you have other resources to share, reach out.
Email ’em to me, other people I should interview. I would love to hear it. Thanks again to my guest, Jessica EO. And tell us again the website that mainly the pieces you’re discussing can be found on
Jessica Empeño: Compassion and choices.org is a great place to start.
Diane Hullet: Beautiful. And as always, you can find out more about the work I do at bestlifebestdeath.com. Thanks so much for listening.

End of Life Doula, Podcaster, and founder of Best Life Best Death.